What is intervertebral disc disease?
Intervertebral disc disease is the most common disease of the spine in dogs (much less common in cats).
Intervertebral discs are fibrocartilage structures between the vertebrae that allow micromovement and act as shock absorbers. They consist of a fibrous outer ring (anulus), and jelly-like core (nucleus).

OpenStax College, CC BY 3.0, via Wikimedia Commons
Degeneration of the intervertebral discs leads to changes in the histological structure that reduce their elastic properties.
The end result can be a “rupture” of disc material (disc herniation) and compression of the spinal cord.

Laboratoires Servier, CC BY-SA 3.0, via Wikimedia Commons
What causes intervertebral disc disease and which breeds are predisposed?
Some breeds (chondrodystrophoid) are genetically predisposed to intervertebral disc degeneration. In them, changes (dehydration) in the structure of the connective tissue begins at an early age
Such are young (up to 5-6 years old) small breeds of dogs as Dachshund, Basset hound, Japanese hin, lhasa apso, Shih tzu, Pekingese, Cocker spaniel, and others. The reason for this is that they were genetically selected for the exterior of “dwarf dogs” and most of these dogs have a long body and short limbs.
Unfortunately, exterior selection has led to a defect in the development of cartilage of the entire skeleton, including the intervertebral discs.
An abnormal elasticity of the discs in them, can lead to disc herniation and compression of the spinal cord.

There are three types of disc herniation- Hansen I, Hansen II и Hansen III.
Acute disc herniation (Hansen type I, extrusion)
Small breeds of dogs at a young age (between 2 and 6 years) are most often affected. Larger breeds are very rarely affected.
Clinical signs usually appear suddenly.
Disc herniation is most easily described as „extrusion“ or leakage of the internal contents of the intervertebral disc.
When the disc changes, it loses its stability and even normal movements (especially torsion) lead to its rupture. Unfortunately, this is always to the vertebral canal, therefore compressing the spinal cord.
The speed of extrusion and the volume of the ruptured disc affect the severity of the spine damage.
The severity of the clinical signs varies from pain syndrome to complete paralysis.
Severe cases of herniated disc (Hansen type I) are an emergency that requires prompt consultation with a veterinary surgeon.
"Disc Disease" (Hansen type II, protrusion)
This disease is similar to disc disease in humans. Instead of extrusion of the center of the disc, there is a prolapse (protrusion) of the periphery.
Unlike acute rupture, the symptoms usually develop more slowly and progressively. Larger breeds of dogs (German Shepherd, hunting breeds), at a later age of 5-12 years, are relatively more often affected.

Laboratoires Servier, CC BY-SA 3.0, via Wikimedia Commons
Traumatic disc herniation, Hansen type III - acute noncompressive hernia
The cause of this type of hernia is a specifically directed spinal cord trauma, which leads to an explosive loss of the normal disc nucleus in the event of a sudden traumatic rupture of the ring (annulus). A small amount of normal disc material injures the spinal cord without subsequent compression.
Clinical signs are usually paralysis and pain.
The prognosis varies, and in mild to moderate cases, improvement is possible with rehabilitation and physiotherapy without surgery.
In severe cases, myelomalacia (a necrotic process in the spinal cord) can develop, which can be fatal.
How a ruptured disc affects the spinal cord?
Figuratively, the spinal cord is very similar to a cable, which consists of thousands of small wires. When pressed, the transmission of information through the many microscopic threads is disrupted.
In a herniated disc, the nucleus is pushed up and compresses the spinal cord or the nerves that come out of it.
Pressure on the nerve root results in varying degrees of acute pain (nerve root signature), and if enough disc material has been expulsed into the canal, the spine is compressed and neurological deficit develops.


Is a sudden onset possible?
Disc degeneration occurs relatively slowly - for weeks and months, but the disc herniation itself usually develops very quickly.
Some dogs develop severe paralysis within an hour. The faster the onset, the greater is the need of emergency veterinary care.
How can I tell if my dog has a herniated disc?
The most common symptom is back or neck pain.
In addition to vocalization, common signs are unusual posture (head bowed), trembling, rapid breathing, reluctance to move, difficulty ascending and descending furniture / stairs.
In more severe cases, there may be difficulty walking, ranging from weakness to complete paralysis.
The most severe cases are those with paralysis, lack of bladder control and loss of sensation.
If the paralysis affects all four limbs, the disc hernia is in the neck area.

How to diagnose a herniated disc?
The first guideline is a history of pain, incoordination, or paralysis without a history of trauma.
Clinical examination usually reveals whether there is a neurological deficit of the spinal cord.
Another important detail is the breed of the patient. If the dog is one of the predisposed breeds, the diagnosis is even more likely.
In some cases, a simple (plain) x-ray may help localize the problem, but the results can be misleading. The normal and often the degenerated disc are X-ray-negative.
When the patient needs surgery and the plain radiography fails to detect the problem, it is necessary to use more advanced diagnostic imaging tools - contrast examination (myelography), computed tomography (scanner) or magnetic resonance imaging.


What are the degrees of neurological deficit?
First degree is characterized by mild pain and is usually self-limiting within few days.
Second degree causes moderate to severe pain that persists longer.
Third degree partial paralysis (paresis) and incoordination of movements.

A 2-year-old French bulldog with third-degree neurological deficit due to an acute disc herniation.
In grade four, there is paralysis (inability to stand up), but with deep sensitivity.

Fourth degree neurological deficit
The most severe, fifth degree is characterized by complete paralysis and lack of deep sensitivity.
Switching from one stage to another can take place within an hour or a day.

7-year-old Dachshund with fifth-degree neurological deficit.
With a strong stimulus, the dog does not turn around and does not feel anything.
Lacks deep sensitivity.
When is conservative therapy applied?
Drug treatment can be used in patients with pain syndrome or in patients with mild deficiency. Less commonly, this therapy may be successful in more severe cases.
Dogs that have lost their sense of deep pain need urgent (within hours) surgery.
The disadvantages of conservative treatment are more frequent recurrence of clinical signs and a greater chance of permanent neurological deficit.
The most important element of conservative therapy is restriction of movement (cage rest).
Restricting the patient's movements can prevent further extrusion of disc material.
The body's natural regenerative potential can lead to self-healing of the spinal cord.
When is surgery required?
Patients with neurological deficits (paresis) may need surgery (decompression) because the prognosis is statistically much better than with conservative treatment.
In general, surgical treatment leads to faster recovery and less likelihood of recurrence.
Cases with loss of deep sensitivity (paralysis) definitely require urgent surgery and have worse prognosis.


What is the success rate in treating disc herniations with or without surgery?
| Degree and duration |
Recovery |
| Without surgery |
With surgery |
| II degree up to 1 week: |
80-90 % |
90-95 % |
| II degree over 1 week: |
60-70 % |
90-95 % |
| III degree: |
30-40 % |
85-95 % |
| IV degree up to 3 days: |
< 25 % |
85-95 % |
| IV degree over 3 days: |
< 20 % |
60-70 % |
| V degree up to 24 hours: |
< 5 % |
50 % |
| V degree over 24 hours: |
< 5 % |
20 % |
| V degree over 72 hours: |
< 5 % |
< 5 % |
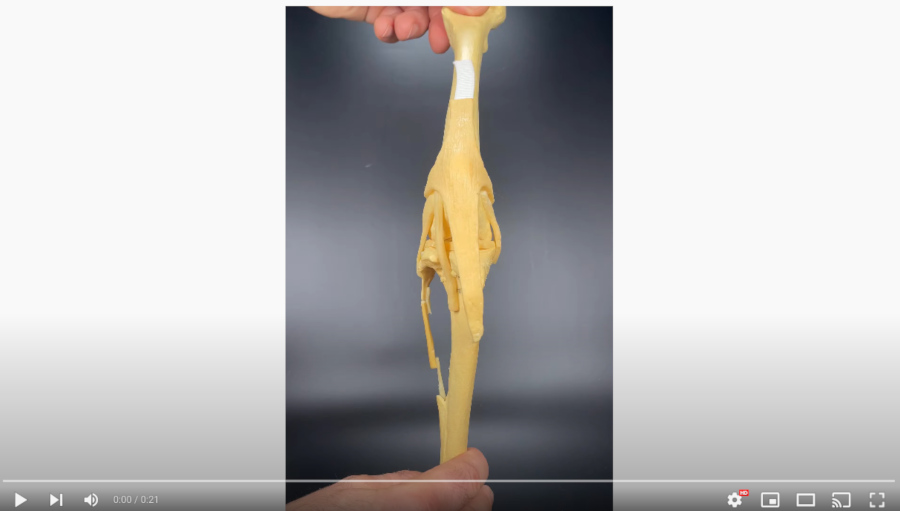
What does the operation involve?
The most commonly used is decompressive surgery in which the ruptured disc material is removed from the spinal canal.
The specific surgery technique depends on the location of the problem.
In the neck area, a ventral approach is preferred or the so-called "ventral slot".


In the thoracolumbar region, the so-called "hemilaminectomy" is most commonly performed.


For lumbosacral problems, dorsal laminectomy is used, in which, figuratively speaking, "the roof" of the canal in the area is removed, which allows direct visualization of the end of the spinal nerves.

A particular challenge is the treatment of chronic disc herniation (protrusions). They require a more technically complex intervention - a corpectomy, which removes a small part of the vertebral body.


When can my dog go home after surgery?
The duration of the postoperative stay in the clinic varies depending on the level of comfort (pain), functional status and control of urination.
How long do patients recover from surgery?
The rate of recovery is individual, as it depends on the severity and duration of spinal compression. The mildest cases recover in days, the more severe in weeks.
Unfortunately, in some cases, permanent deficits that do not improve over time are possible.
Postoperative physiotherapy can significantly accelerate the rate of recovery of patients with paresis.

Are there solutions if my dog doesn't regain his neurological function?
Many dogs can continue to enjoy life with wheelchairs.
However, these patients require daily help to empty their bladder.
Paralyzed patients can evacuate their bladder with the help of the owners (manual compression in the area). The technique is not difficult and can be easily mastered with the help of demonstration and practice.

Can the problem recur?
With a well-performed spinal operation, it is very unusual to have a problem with the same disc. However, degeneration of any of the other disks is possible.
Up to 10% of patients may have a second serious problem that requires surgery.
Is there prevention?
There is no proven method to reduce the likelihood of developing disc disease (including dietary supplements).
Keeping the patient in good physical condition is always useful in diseases of the musculoskeletal system.
In the event of degenerative changes in the discs, it is possible to perform preventive surgery (so-called fenestration), which has been shown to reduce the chance of acute prolapse of the affected disc.
doctorzlatinov.com/EN/#article-30

 AO VET Dubrovnik, 2017
AO VET Dubrovnik, 2017  AO VET Lisbon, 2019
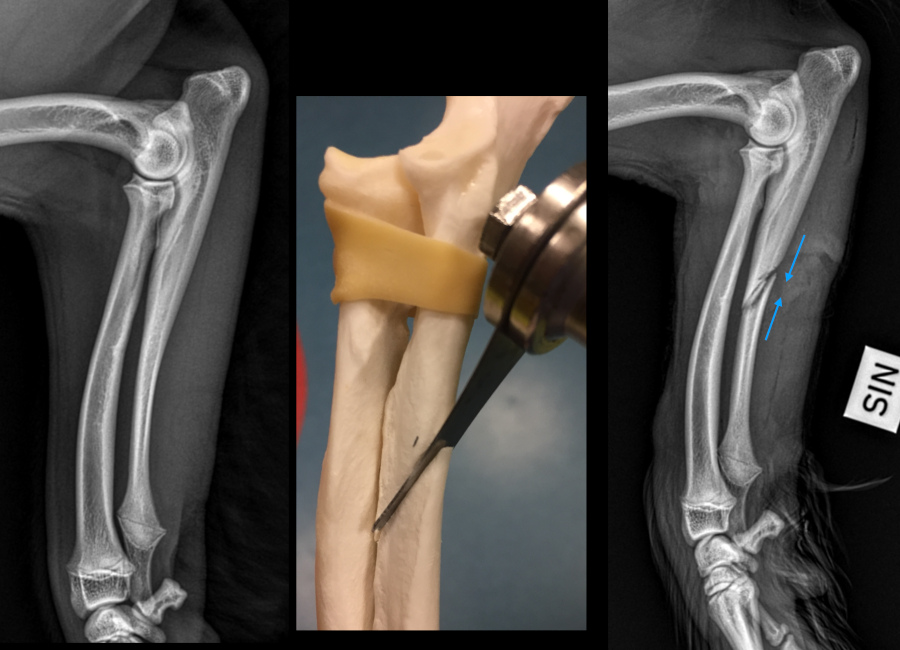
AO VET Lisbon, 2019  BAVOT, 2019, corrective osteotomy of the hindlimb
BAVOT, 2019, corrective osteotomy of the hindlimb  BAVOT, seminar with Mike Farrell and Ignacio Calvo, 2018
BAVOT, seminar with Mike Farrell and Ignacio Calvo, 2018  BAVOT, seminar with Prof. Bruno Peyrone
BAVOT, seminar with Prof. Bruno Peyrone  Intrauma symposium, 2019
Intrauma symposium, 2019  Leon Congress, Mexico, 2019
Leon Congress, Mexico, 2019  AO VET, Pan-Asian Conference, 2019
AO VET, Pan-Asian Conference, 2019  TPLO workshop with Massimo Petazzoni, 2017
TPLO workshop with Massimo Petazzoni, 2017  VOG seminar, Croatia, 2016
VOG seminar, Croatia, 2016